- Thoracic Spine Decompression
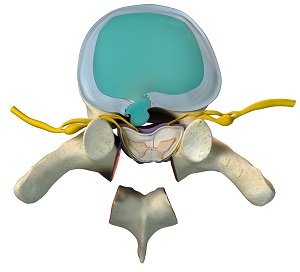
Thoracic spine decompression is a procedure to relieve pressure on the spinal nerves in the middle portion of the back. Spine decompression surgery is indicated in treating spinal stenosis.
Know More - Thoracic Spine Fusion
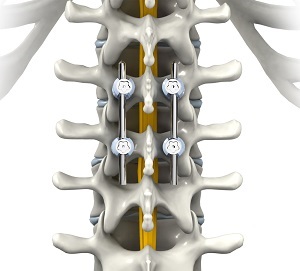
Thoracic spine fusion is a surgical procedure in which two or more bones (vertebrae) of the thoracic spine are joined together to eliminate the movement between them.
Know More - Thoracic Vertebroplasty

Osteoporosis is a “silent” disease characterized by weakening of bones, making them more susceptible to fractures, typically in the hip and spine. Elderly people and especially post-menopausal women are at greater risk of developing osteoporosis.
Know More - Thoracic Discectomy
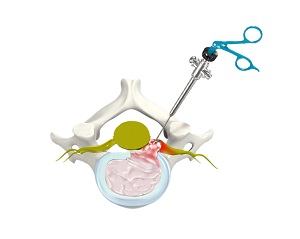
The human spine provides support to the body allowing you to stand upright, bend, and twist. The spine can be broadly divided into cervical, thoracic and lumbar spine.
Know More

The Spine Clinic of Oklahoma City
9800 Broadway Ext
Oklahoma City, OK 73114
Dr. Braly: Suite 203
Dr. Beacham: Suite 201
9800 Broadway Ext
Oklahoma City, OK 73114
Dr. Braly: Suite 203
Dr. Beacham: Suite 201
