- Lumbar Fusions
Spinal fusion, also called arthrodesis, is a surgical technique used to join two or more vertebrae (bones) within the spine. Lumbar fusion technique is the procedure of fusing the vertebrae in lumbar portion of the spine (lower back).
Know More - Lumbar Artificial Disc Replacements

Lumbar artificial disc replacement is a surgical method of replacing the diseased or damaged intervertebral discs of the spinal column with an artificial disc to restore motion to the spine.
Know More - Minimally Invasive Lumbar Fusions
Spinal fusion is a surgical technique used to join two or more vertebrae in the spine and to minimize the pain caused by movement of these vertebrae.
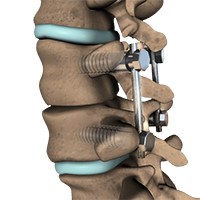
Know More - Posterior Lumbar Fusions
Spinal fusion, also called arthrodesis, is a surgical technique used to join two or more vertebrae (bones) within the spine. Lumbar fusion technique is the procedure of fusing the vertebrae in lumbar portion of the spine (lower back).
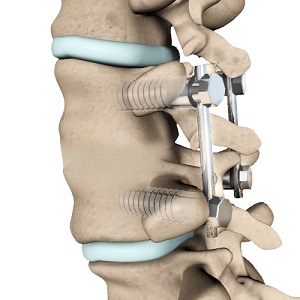
Know More - Posterior Lumbar Interbody Fusion Surgery

Spinal fusion is a surgical technique used to join two or more vertebrae in the spine and to minimize the pain caused by movement of these vertebrae. Fusion of vertebrae in lumbar portion of the spine is called as lumbar fusion and the surgery can be done as an open or minimally invasive procedure.
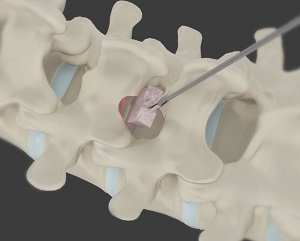
Know More - Posterolateral Lumbar Fusion
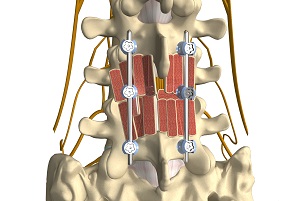
Posterolateral lumbar fusion is a surgical technique that involves correction of spinal problems from the back of the spine by placing bone graft between segments in the back and leaving the disc space intact.
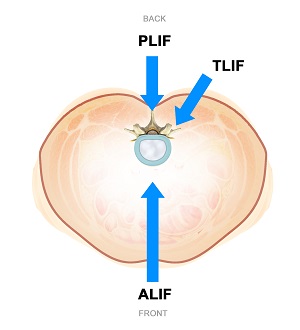
Know More - Transforaminal Lumbar Interbody Fusion (TLIF)

Transforaminal lumbar interbody fusion (TLIF) is a type of spinal fusion procedure in which bone graft is placed between the affected vertebrae in the lower back (lumbar) region through an incision on the patient’s back.
Know More - Minimally Invasive Lumbar Discectomy
Lumbar discectomy is a spinal surgery that involves removal of damaged intervertebral disc to relieve pressure on the spinal nerves (decompression) in the lumbar (lower back) region.
Know More - Lumbar Microdiscectomy
Microdiscectomy is a surgical procedure employed to relieve the pressure over the spinal cord and/or nerve roots, caused by a ruptured (herniated) intervertebral disc.
Know More - Lumbar Laminectomy

Lumbar laminectomy, also known as decompression laminectomy, is a spinal surgery done to relieve excess pressure on the spinal nerve(s) in the lumbar (lower back) region.
Know More Launch Movie - Anterior Lumbar Corpectomy and Fusion

Anterior Lumbar Corpectomy and Fusion is a surgical technique performed to remove the vertebral bone or disc material between the vertebrae to alleviate pressure on the spinal cord and spinal nerves (decompression) in the lumbar (lower back) region.
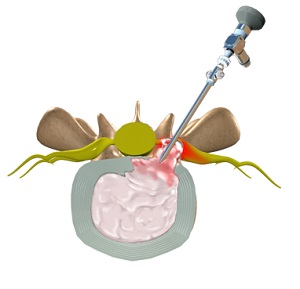
Know More - Lumbar Discectomy

Intervertebral discs are fibrocartilaginous cushions between adjacent vertebrae in the spine. The normal intervertebral disc is composed of a semi-liquid substance (nucleus pulposus) at the center surrounded by a fibrous ring (annulus fibrosis).
Know More - X-LIF Extreme Lateral Interbody Fusion

Extreme lateral interbody fusion (XLIF) is a minimally-invasive surgery that involves the fusing of two degenerative spinal vertebrae. The procedure is conducted to relieve painful motion in the back caused by spinal disorders.
Know More

The Spine Clinic of Oklahoma City
9800 Broadway Ext
Oklahoma City, OK 73114
Dr. Braly: Suite 203
Dr. Beacham: Suite 201
9800 Broadway Ext
Oklahoma City, OK 73114
Dr. Braly: Suite 203
Dr. Beacham: Suite 201
