- Herniated Disc (Lumbar)
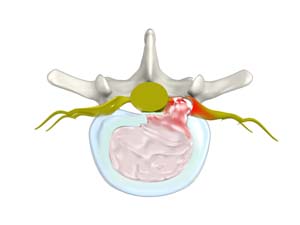
Herniated disc is a condition in which the outer fibers (annulus) of the intervertebral disc are damaged causing the soft inner material of the nucleus pulposus to rupture out of its space. A herniated disc, common in the lower back (lumbar spine) occurs when there is a tear in the outer lining of the disc (annulus fibrosus).
Know More - Lumbar Stenosis

Lumbar stenosis is the compression of spinal nerves caused by narrowing of spinal canal and it is one of the common causes of low back pain. Spinal stenosis can also affect the spine in neck region. The symptoms include back pain, burning or aching type of pain in buttocks that radiates to the legs (sciatica), weakness in the legs or "foot drop".
Know More - Back Pain

Back pain or backache is the pain felt in the back that may originate from muscles, nerves, bones, joints or other structures in the spine. Back pain is one of the most common medical problems experienced by most people at some time in their life.
Know More - Sciatica
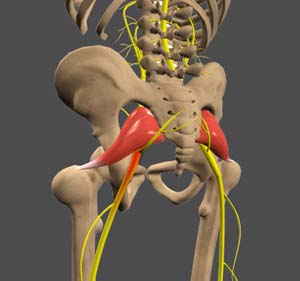
The sciatic nerve is a large nerve that originates in the lower back, running along the hip and back of the leg and branching off at the knee. Compression or damage of this nerve can cause pain that radiates from your lower back to the buttocks, to your legs.
Know More

The Spine Clinic of Oklahoma City
9800 Broadway Ext
Oklahoma City, OK 73114
Dr. Braly: Suite 203
Dr. Beacham: Suite 201
9800 Broadway Ext
Oklahoma City, OK 73114
Dr. Braly: Suite 203
Dr. Beacham: Suite 201
